Secondary fracture prevention: consensus clinical recommendations from a multistakeholder coalition
Prevence sekundárních fraktur: multioborové konsenzuální stanovisko ke klinickým doporučením
Fraktury související s osteoporózou jsou v současnosti nedostatečně léčeny („podléčeny“), a to z části pro mylné informace o doporučených postupech v péči o pacienty a z části pro rozdíly v doporučeních pro léčbu. Aby se zvrátil tento nevyhovující stav a zlepšily se léčebné výsledky pacientů, sestavila Americká společnost pro výzkum kostí a kostního minerálu širokou skupinu zainteresovaných odborníků ke koncipování klinických doporučení k optimalizaci prevence sekundárních fraktur v populaci osob ve věku 65 let a starších postižených frakturami krčku kosti stehenní nebo obratlů. Tato skupina připravila 13 doporučení (7 primárních a 6 sekundárních) přesvědčivě potvrzených důkazy z odborné literatury. Skupina doporučuje rozšíření a zintenzívnění komunikace s pacienty o problematice rizika fraktur, o mortalitní i morbiditních dopadech fraktur stejně jako o možnostech snížení tohoto rizika. Podle odhadu se může riziko (včetně pádů) objevovat v pravidelných intervalech v závislosti na fyzioterapii nebo ergoterapii, což je očekávatelné. Perorálně, intravenózně i subkutánně aplikované léky jsou účinné a mohou snížit riziko fraktur. Pacienti samozřejmě potřebují edukaci o přínosech i rizicích těchto různě aplikovaných léků, stejně jako o důsledcích neléčení. Perorální bisfosfonáty alendronát a risendronát představují léčbu první volby a jsou všeobecně dobře tolerovány; možné je zvážit i intravenózně podávanou kyselinu zoledronovou nebo subkutánně podávaný denosumab. Anabolika jsou nákladná, ale mohou být pro vybrané pacienty ve vysokém riziku přínosná. Optimální délka farmakoterapie není známa, ale protože je riziko sekundárních fraktur v raném období po fraktuře velmi vysoké, doporučuje se bezodkladná léčba. Samozřejmostí by měla být adekvátní dieta, případně suplementace vitamínem D stejně tak by měl být samozřejmostí přísun kalcia. Jednotlivci léčení na osteoporózu by měli být běžně opakovaně vyšetřováni vzhledem k riziku fraktur a opakovaně informování v rámci pacientské edukace o osteoporóze a riziku fraktur a o monitorování nežádoucích účinků léčby. Pacienti by měli být důrazně přesvědčováni, aby se vyvarovali kouření a co možná nejvíce omezili konzumaci alkoholu, věnovali se pravidelně fyzické aktivitě a přijali a dodržovali strategie prevence. Závěrem doporučení upozorňuje endokrinology a ostatní odborníky na osteoporózu, aby věnovali pozornost jedincům s opakovanými frakturami anebo úbytkem kostní hmoty a také jedincům s komplikujícími komorbiditami (např. hyperparatyreoidizmus nebo chronické onemocnění ledvin).
Klíčová slova:
stárnutí – anabolika – antirezorptiva – osteoporóza – sekundární fraktura prevence
Authors:
Conley B Robert 1; Adib Gemma 2; Robert; Adler 3; Kesson E Kristina 4; Alexander M Ivy 5; Amenta C Kelly 6; Blank D Robert 7,8; Brox Timothy William 9; Carmody E Emily 10; Chapman-Novakofski Karen 11; Clarke L Bart 12; Cody M Kathleen 13; Cooper Cyrus 14; Crandall J Carolyn 15; Dirschl R Douglas 16; Eagen J Thomas 17; Elderkin L Ann 18; Fujita Masaki 19; Greenspan L Susan 20; Halbout Philippe 21; Hochberg C Marc 22; Javaid Muhammad 23; Jeray J Kyle 24; Kearns E Ann 12; King Toby 25; Koinis F Thomas 26; Koontz Scott Jennifer 27,28; Kužma Martin 29; Lindsey Carleen 30; Lorentzon Mattias 31,32,33; Lyritis P George 34; Michaud Boehnke Laura 35; Miciano Armando 36; Morin N Suzanne 37; Mujahid Nadia 38; Napoli Nicola 39,40; Olenginski P Thomas 41; Puzas Edward J 10; Rizou Stavroula 34; Rosen J Clifford 42,43; Saag Kenneth 44; Thompson Elizabeth 45; Tosi L Laura 46; Tracer Howard 47; Khosla Sundeep 12; Kiel P Douglas 48
Authors place of work:
Center for Medical Technology Policy, Baltimore, MD, USA
1; Osteoporosis Centre, Damascus, Syria
2; McGuire VA Medical Center, Richmond, VA, USA
3; Lund University and Skåne University Hospital, Lund, Scania, Sweden
4; UConn School of Nursing, University of Connecticut, Storrs, CT, USA
5; Department of Physician Assistant Studies, Mercyhurst University, Erie, PA, USA
6; Department of Endocrinology, Metabolism and Clinical Nutrition, Medical College of Wisconsin, Milwaukee, WI, USA
7; Garvan Institute of Medical Research, Darlinghurst, NSW, Australia
8; UCSF Fresno, Fresno, CA, USA
9; Department of Orthopaedics and Rehabilitation, University of Rochester Medical Center, Rochester, NY, USA
10; Division of Nutritional Sciences, University of Illinois, Urbana, IL, USA
11; Division of Endocrinology, Diabetes, Metabolism, Nutrition, Department of Internal Medicine, Mayo Clinic, Ro-chester, MN, USA
12; American Bone Health, Raleigh, NC, USA
13; University of Southampton, Southampton, UK
14; Department of Medicine, University of California, Los Angeles, CA, USA
15; Department of Orthopaedic Surgery and Rehabilitation Medicine, University of Chicago Medicine, Chicago, IL, USA
16; National Council on Aging, New York, NY, USA
17; American Society for Bone and Mineral Research, Washington, DC, USA
18; Science Department, International Osteoporosis Foundation, Nyon, Switzerland
19; Department of Medicine, University of Pittsburgh, Pittsburgh, PA, USA
20; International Osteoporosis Foundation, Nyon, Switzerland
21; Division of Rheumatology, University of Maryland School of Medicine and VA Maryland Health Care System, Baltimore, MD, USA
22; Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences, University of Oxford, Oxford, USA
23; Prisma Health Upstate (formerly Greenville Health System), Greenville, SC, USA
24; US Bone and Joint Initiative, Rosemont, IL, USA
25; Duke Primary Care Oxford, Oxford, NC, USA
26; Orthopedics & Sports Medicine, Newton Medical Center, Newton, KS, USA
27; Department of Family and Community Medicine, University of Kansas School of Medicine, Wichita, KS, USA
28; Bones, Backs and Balance, LLC, Bristol Physical Therapy, LLC, Bristol, CT, USA
30; Mary MacKillop Institute for Health Research, Australian Catholic University, Melbourne, Victoria, Australia
31; Department of Geriatric Medicine, Sahlgrenska University Hospital, Mölndal, Sweden
32; Geriatric Medicine, Institute of Medicine, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden
33; Hellenic Osteoporosis Foundation, Athens, Greece
34; The University of Texas MD Anderson Cancer Center, Houston, TX, USA
35; Nevada Rehabilitation Institute, Las Vegas, NV, USA
36; Department of Medicine, McGill University, Montreal, Canada
37; Department of Medicine, Warren Alpert Medical School, Brown University, Providence, RI, USA
38; Department of Nutrition and Metabolic Disorders, Campus Bio-Medico University of Rome, Rome, Italy
39; Department of Medicine, Washington University School of Medicine, St. Louis, MO, USA
40; HiROC Program/Rheumatology, Geisinger Health System, Danville, PA, USA
41; Tufts University School of Medicine, Boston, MA, USA
42; Maine Medical Center Research Institute, Portland, ME, USA
43; Division of Clinical Immunology and Rheumatology, University of Alabama at Birmingham, Birmingham, AL, USA
44; National Osteoporosis Foundation, Arlington, VA, USA
45; Department of Orthopaedic Surgery and Sports Medicine, Children’s National Hospital, Washington, DC, USA
46; Center for Evidence and Practice Improvement, Agency for Healthcare Research and Quality, Rockville, MD, USA
47; Harvard Medical School, Musculoskeletal Research Center, Marcus Institute for Aging Research, Hebrew Senior Life, Boston, MA, USA
48; th Department of Internal Medicine, University Hospital, Comenius University, Bratislava, Slovakia
295
Published in the journal:
Clinical Osteology 2020; 25(1): 7-25
Category:
Doporučené postupy
Summary
Osteoporosis-related fractures are undertreated, due in part to misinformation about recommended approaches to patient care and discrepancies among treatment guidelines. To help bridge this gap and improve patient outcomes, the American Society for Bone and Mineral Research assembled a multistakeholder coalition to develop clinical recommendations for the optimal prevention of secondary fracture among people aged 65 years and older with a hip or vertebral fracture. The coalition developed 13 recommendations (7 primary and 6 secondary) strongly supported by the empirical literature. The coalition recommends increased communication with patients regarding fracture risk, mortality and morbidity outcomes, and fracture risk reduction. Risk assessment (including fall history) should occur at regular intervals with referral to physical and/or occupational therapy as appropriate. Oral, intravenous, and subcutaneous pharmacotherapies are efficacious and can reduce risk of future fracture. Patients need education, however, about the benefits and risks of both treatment and not receiving treatment. Oral bisphosphonates alendronate and risedronate are first-line options and are generally well tolerated; otherwise, intravenous zoledronic acid and subcutaneous denosumab can be considered. Anabolic agents are expensive but may be beneficial for selected patients at high risk. Optimal duration of pharmacotherapy is unknown but because the risk for second fractures is highest in the early post-fracture period, prompt treatment is recommended. Adequate dietary or supplemental vitamin D and calcium intake should be assured. Individuals being treated for osteoporosis should be reevaluated for fracture risk routinely, including via patient education about osteoporosis and fractures and monitoring for adverse treatment effects. Patients should be strongly encouraged to avoid tobacco, consume alcohol in moderation at most, and engage in regular exercise and fall prevention strategies. Finally, referral to endocrinologists or other osteoporosis specialists may be warranted for individuals who experience repeated fracture or bone loss and those with complicating comorbidities (eg, hyperparathyroidism, chronic kidney disease).
Keywords:
osteoporosis – aging – anabolics – antiresorptives – secondary fracture prevention
Introduction
There has been a growing recognition in recent years that, despite remarkable advances in our understanding of the pathogenesis and treatment of osteoporosis, many patients who warrant pharmacological treatment for the prevention of fractures are either not being offered treatment or are opting not to take medications such as bisphosphonates or other osteoporosis drugs [1,2]. Although one of the reasons for this undertreatment clearly stems from concerns regarding rare side effects of osteoporosis medications, particularly bisphosphonates, other reasons persist as well (e.g. discrepancies among treatment guidelines) [2]. Recognizing this widening “treatment gap,” the American Society for Bone and Mineral Research (ASBMR) engaged the Center for Medical Technology Policy (CMTP) to help develop a consensus of a broad multistakeholder coalition regarding several aspects of osteoporosis treatment. The first, and perhaps most critical, decision the coalition made was to target this effort to a group where there was little controversy that the benefits of treatment almost always outweighed the risks – people aged 65 years or older with a hip or vertebral fracture [3]. By focusing its clinical recommendations on secondary prevention, the coalition sought not only to unequivocally target high-risk patients but also to establish a “floor” upon which subsequent treatment strategies could be built. The following recommendations are unique in the field because they were developed and supported by professionals from all segments of the osteoporosis treatment community and provide a workable base for building future consensus.
Methodology
Based on a review of existing clinical guidelines and medical literature, CMTP developed an initial set of draft recommendations, which were reviewed and edited by the coalition co-chairs and ASBMR, the coalition Steering Committee, and the full coalition, sequentially. The cycle was repeated until consensus was reached. The same process was followed to develop accompanying text that provided rationales, more detailed explanations, and supporting references. After the coalition reached agreement on the full document, a technical/scientific editor was hired to condense the paper into an abbreviated manuscript appropriate for publication.
Although the recommendations do not include explicit assessment of the quality of supporting evidence, one of the coalition’s fundamental principles was to follow the evidence and focus where the data are strongest. Because disagreements seem to occur most frequently when the scientific evidence is lacking or contradictory, we believed that consensus could be achieved even within a very diverse coalition by concentrating efforts where the evidence is clear and strong. Where coalition members have substantially disagreed about the propriety of a proposed recommendation, we generally either removed the recommendation or stated that the most appropriate action is not known and then elaborated on the point in the accompanying text. The recommendations would lose credibility if they adopted strong positions on controversial issues based on opinion rather than on convincing evidence.
Scope and purpose of the recommendations
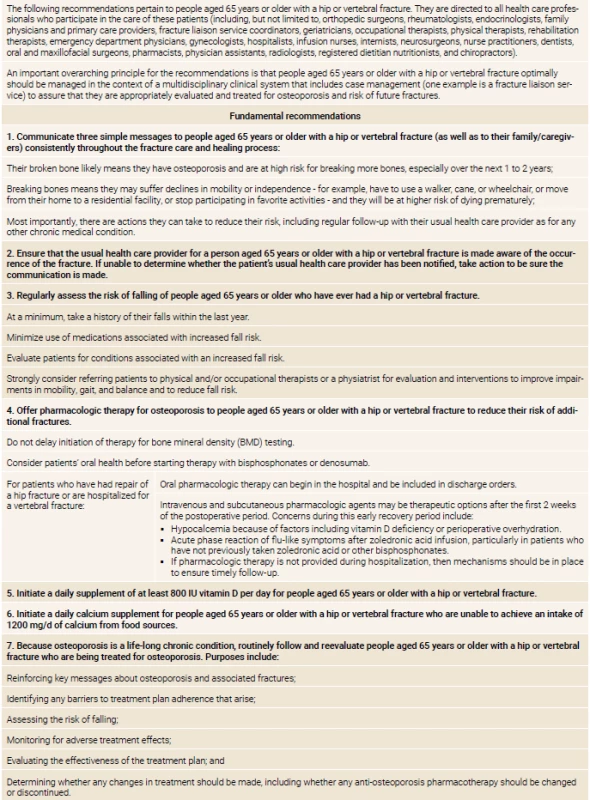
Consensus recommendations are summarized in table 1 and explicated further in the text that follows. (Coalition member organizations and individuals are listed in table 2). “Consensus” means general agreement, not that every coalition member approves of every specific element.
These recommendations are not intended to address clinical management of acute fractures or how to optimize recovery; such issues are beyond the scope of this document and this initiative. They focus on patients within a certain age range who have experienced certain osteoporotic fractures that come to clinical attention, although it is critical to emphasize that fracture prevention is also needed for other high-risk populations. These recommendations are intended to complement other fracture prevention efforts, not compromise them.
An important overarching principle for the recommendations is that optimal management should occur in the context of a multidisciplinary clinical system that includes case management to assure patients are appropriately evaluated and treated for osteoporosis and risk of future fractures. A substantial, growing body of literature demonstrates that the most effective organizational approach to secondary fracture prevention is a multidisciplinary case management approach that frequently takes the form of a fracture liaison service (FLS) [4–11]. FLS programs are cost-effective or cost-saving in several different practice settings [8], and have been broadly and successfully adopted internationally [12,13]. Although there may be settings where FLS programs cannot be fully implemented, the coalition strongly recommends that institutions attempt to establish them. Several organizations, including the American Orthopaedic Association’s Own the Bone [14], the National Osteoporosis Foundation [15], and the International Osteoporosis Foundation’s Capture the Fracture [16], have developed resources to assist with establishing and sustaining FLSs [14–18].
Finally, these recommendations are intended to be used as general guidance only and are specific to clinical situations in the United States (US). They may not apply to all patients in all circumstances and in other countries, and they are not meant to replace clinical judgment and management decisions reached through informed discussions with patients.
Fundamental recommendations and rationales
Recommendation 1: Communicate three simple messages to people aged 65 years or older with a hip or vertebral fracture (as well as to their family/caregivers) consistently throughout the fracture care and healing process:
Their broken bone likely means they have osteoporosis and are at high risk for breaking more bones, especially over the next 1 to 2 years;
Breaking bones means they may suffer declines in mobility or independence – for example, have to use a walker, cane, or wheelchair, or move from their home to a residential facility, or stop participating in favorite activities – and they will be at higher risk of dying prematurely;
Most importantly, there are actions they can take to reduce their risk, including regular follow-up with their usual health care provider as for any other chronic medical condition.
Hip or vertebral fracture in people aged 65 years or older is diagnostic for osteoporosis in the absence of another metabolic bone disease, regardless of bone mineral density (BMD), and is one of the strongest risk factors for subsequent fractures [4,19–21]. The risk of subsequent fracture is significantly elevated, especially in the first 1 to 2 years after a fracture, for all patients – even those with high/normal BMD [22–24].
The impact of hip fractures on physical functioning is substantial. Approximately half of hip fracture patients who survive to 1 year do not regain their prior functionality [25] nor does their health status return to prefracture levels [26]. Only about one-third to one-half of hip fracture survivors regain prior ambulatory function [27–29], and around 13% may be unable to ambulate at all [30]. Of patients surviving 1 year who needed no walking aids prior, approximately 40% require assistance [30].
Loss of autonomy and independence is also reflected in changes of residential settings after fracture. Among more than 43,000 Medicare patients who experienced a hip fracture between 2005 and 2010, 20% of patients who had been living in the community had moved into long-term care at 1 year after fracture [25]. Furthermore, because of the expense of long-term care in the US, 80% of those patients became destitute [25]. Finally, the 1-year mortality for hip-fracture patients ranges from 15% to 30% for community-dwelling residents [25,27,31] to 40% to 55% for long-term care facility residents [25,31].
Most patients do not realize, that they are at risk for another fracture, that osteoporosis caused their fracture, and that interventions can reduce their risk [32]. Thus, they are not likely to take appropriate steps to address their risk [33]. To communicate risk related messages effectively, all health care professionals should provide consistent and sustained messaging throughout the care pathway, beginning at time of diagnosis and continuing repeatedly [4,5]. These messages also should be communicated to family/caregivers. Providing key information to persons who will be involved with patients’ care will increase the likelihood that patients receive it. Mentioning how patients can reduce their risk provides a positive message and sets the stage for additional counseling and interventions. Emphasizing the connection between fracture and osteoporosis elevates the fracture from an unfortunate accident to a sentinel event indicative of an important underlying chronic disorder.
Recommendation 2: Ensure that the usual health care provider for a person aged 65 years or older with a hip or vertebral fracture is made aware of the occurrence of the fracture. If unable to determine whether the patient’s usual health care provider has been notified, take action to be sure the communication is made.
Lack of communication with patients’ usual health care providers has consistently been identified as one of the key barriers to providing appropriate management for secondary fracture prevention [4]. Many patients do not understand the long-term significance and importance of their fracture. If usual health care providers are not aware of the occurrence of a fracture and the diagnosis of osteoporosis, they cannot take steps to provide the long-term care that this lifelong, chronic condition requires. Vertebral fractures, in particular, are seldom noted in medical records and reports and, if they are mentioned, are often reported with ambiguous or confusing terminology [34–38]. Additionally, patients are at highest risk for another fracture in the months immediately after the initial hip or vertebral fracture [39], and steps need to be taken on an urgent basis to reduce that risk. When unable to determine whether the patient’s usual health care provider has been notified, sufficient action might entail calling the provider or sending an email or letter. Documenting the action in the patient’s medical record ensures better continuity of care.
Recommendation 3: Regularly assess the risk of falling of people aged 65 years or older who have ever had a hip or vertebral fracture.
At a minimum, take a history of their falls within the last year.
Minimize use of medications associated with increased fall risk.
Evaluate patients for conditions associated with an increased fall risk.
Strongly consider referring patients to physical and/or occupational therapists or a physiatrist for evaluation and interventions to improve impairments in mobility, gait, and balance and to reduce fall risk.
About one-third of community-dwelling persons aged 65 years or older fall each year, with the incidence steadily increasing until age 80 years [40,41]. Up to 15% of falls in older adults result in fractures [40,41] and around 90% of hip fractures result from a simple fall from standing height or less [42,43]. Consequently, several entities, including the Centers for Disease Control and Prevention, stress that the best way to prevent hip fractures is through preventing falls [44–47]. Just as having had one osteoporotic fracture is one of the best predictors of having another fracture, having had a previous fall is one of the best predictors of having another fall [48]. For this reason, asking patients about their history of falls should routinely be part of caring for patients with osteoporosis [21,48,49].
Particular medication classes associated with higher chance of falling are often referred to as fall-risk-increasing drugs (FRIDs). These include loop diuretics, antipsychotics, antidepressants, benzodiazepines, antiepileptics, and opioids [50–52]. Fall risk may vary with the particular agent, however; thus, short-acting benzodiazepines and selective serotonin reuptake inhibitors may be safer in terms of fall risk than other drugs within their categories [51], and the selectivity of beta-blockers may be a relevant factor [50]. Pharmacists can be helpful in reviewing FRID us and recommending potential alternatives associated with lower risk of falls. Although the association between fall risk and FRIDs is clear and it would seem logical that minimizing FRID use would reduce falls and therefore fractures, the evidence demonstrating this effect is not robust.
Several other risk factors for falls also have been identified, including age; deficits in visual, proprioception, and vestibular systems; decline in lower-extremity physical performance; comorbidity burden; nutritional status; hypoglycemia in patients with type 2 diabetes; fear of falling; and various environmental factors [53–55]. The CDC has published a compendium of 41 effective fall prevention interventions [56] and developed a Stopping Elderly Accidents, Deaths, and Injuries (STEADI) program based on guidelines from the American Geriatric Society and British Geriatrics Society [57,58] that includes a toolkit, algorithm, training videos, and checklists to help clinicians [59]. Additional information on fall prevention is also available through the US Preventive Services Task Force [48] and the National Institutes of Health [60].
Recommendation 4: Offer pharmacologic therapy for osteoporosis to people aged 65 years or older with a hip or vertebral fracture to reduce their risk of additional fractures.
Do not delay initiation of therapy for BMD testing.
Consider patients’ oral health before starting therapy with bisphosphonates or denosumab.
For patients who have had repair of a hip fracture or are hospitalized for a vertebral fracture:
Oral pharmacologic therapy can begin in the hospital and be included in discharge orders.
Intravenous and subcutaneous pharmacologic agents may be therapeutic options after the first 2 weeks of the postoperative period. Concerns during this early recovery period include:
Hypocalcemia because of factors including vitamin D defficiency or perioperative overhydration.
Acute phase reaction of flu-like symptoms after zoledronic acid infusion, particularly in patients who have not previously taken zoledronic acid or other bisphosphonates.
If pharmacologic therapy is not provided during hospitalization, then mechanisms should be in place to ensure timely follow-up.
Because front-line clinicians are often already overextended and are not generally trained in exercise modalities [61], the coalition recommends that they consider referring patients at potential high risk for falls to physical or occupational therapists or to physiatrists for evaluation and intervention. Patients who report fear of falling or imbalance may also benefit from using an assistive device.
Pharmacologic therapy for osteoporosis reduces the risk of fracture in older patients who have already experienced a hip or vertebral fracture. The occurrence of hip or vertebral fracture is sufficient to establish a diagnosis of osteoporosis regardless of BMD, and, therefore, treatment initiation should not be delayed for testing. Risk of subsequent fracture is significantly elevated for patients at all levels of BMD [22,24,62,63] and patients with BMD results that fall outside the “usual” diagnostic parameters for osteoporosis can benefit from pharmacotherapy. Most medical societies and professional organizations urge physicians to offer treatment on the basis of the clinical fracture alone [19–21,49,64,65].
Consider a patient’s oral health before starting pharmacologic therapy because of rare instances of osteonecrosis of the jaw (ONJ) occurring in patients taking bisphosphonates or denosumab for osteoporosis. (Recommendation #10 provides more detailed information about ONJ.) Although the evidence is not robust, it appears that the risk of ONJ can be diminished if any needed oral surgery is completed before initiating antiresorptives [66]. There is no need for a full dental assessment pretherapy, however, except potentially for oncology patients who will be starting high and frequent doses of antiresorptives [67]. For the more typical osteoporosis patient, as noted by the Canadian Association of Oral and Maxillofacial Surgeons, “[d]elaying the initiation of bisphosphonate therapy pending a dental evaluation rarely would seem necessary….” [68].
Patients who have had repair of a hip fracture or are hospitalized for a vertebral fracture can begin taking oral anti-osteoporosis pharmacotherapy in the hospital. Previously, there have been concerns that bisphosphonates might interfere with bone healing and therefore should not be given for some period of time after bone surgery. As evidence has accumulated, however, it has become clear that “[t]he efficacy of bisphosphonates in preventing secondary fractures overwhelms the possible risk of fracture healing impairment associated with the use of bisphosphonates” [69]. Literature reviews and meta-analysis of randomized controlled trials support this conclusion [69–71] and, in the HORIZON trial of intravenous zoledronic acid after hip fracture surgery, no association between zoledronic acid infusion and delayed healing was found, even when patients were provided the drug within the first 2 weeks after surgery [72] (recommendation #11 includes information about how to take oral bisphosphonates that may be particularly relevant for some hospitalized patients.).
Intravenous and subcutaneous anti-osteoporosis pharmacotherapies are associated with other occurrences, however, that can limit their utility in the perioperative period. Intravenous zoledronic acid and subcutaneous denosumab and romosozumab are associated with hypocalcemia [20,73,74], for example, which is a significant risk factor for postoperative delirium in patients undergoing hip fracture repair [75] These drugs are contraindicated in patients with hypocalcaemia [74,76,77], and many surgical patients are hypocalcemic in the postoperative period [78–80]. In the key HORIZON Recurrent Fracture Trial, patients with osteoporosis who had recently fractured a hip did not receive their first zoledronic acid infusion until after they had taken calcium and vitamin D supplements for at least 2 weeks [76,81]. For patients who are severely vitamin D deficient, repletion before providing a strong intravenous or subcutaneous antiresorptive medication may be appropriate.
Patients also can experience, in addition to hypocalcemia, an acute-phase reaction (APR) after infusion of zoledronic acid, characterized primarily by fever and muscle pain. APRs usually occur within the first 3 days after infusion and are most common in patients who have never taken bisphosphonates before and are undergoing infusion for the first time [82,83]. Adequate serum levels of vitamin D may be protective [84], and providing acetaminophen to patients for a few days after the infusion can reduce the incidence of symptoms by around 50%, although it cannot completely eliminate the risk [82,83]. APRs that occur in the hospital are particularly problematic because fever in the perioperative period can also signal infection – they therefore can trigger substantial diagnostic evaluation and potential overtreatment of a suspected infection. Finally, teriparatide and abaloparatide are associated with symptomatic orthostatic hypotension [85,86], which can complicate patient management at a time when encouraging mobility is critical, and therefore should be administered at bedtime while the patient is reclining.
Recommendation 5: Initiate a daily supplement of at least 800 IU vitamin D per day for people aged 65 years or older with a hip or vertebral fracture.
Vitamin D is a critical nutrient that has an important role in calcium absorption and maintenance of serum calcium and phosphate concentrations [79]. Patients with osteoporosis are often vitamin D-deficient [20]. The best single indicator of a patient’s vitamin D status is serum concentration of 25-hydroxy-vitamin D (25(OH)D) [20,87]. because it reflects not only dietary and supplemental vitamin D but also cutaneously produced vitamin D and it has a sufficiently long half-life [87]. The optimal level of 25(OH)D is a matter of controversy, although serum levels in the range of 20 to 30 ng/mL are generally thought to be sufficient. The safe upper limit is also a matter of debate, and there is substantial disagreement over whether to treat to a specified serum level. In the US, the recommended daily allowance of vitamin D is 600 IU for people aged 51 to 70 years and 800 IU for people older than 70 years [87].
The effect of vitamin D alone on the risk of fracture is not clear [19,21], although there is strong evidence that it does reduce fractures when combined with calcium supplements in individuals at high risk of deficiency [21]. It is important to note that the published clinical trials of anti-osteoporosis medications virtually all have involved providing vitamin D and calcium supplements to the enrolled patients, and replicating those treatment regimens is an additional and powerful rationale for recommending supplementation [5,21].
Recommendation 6: Initiate a daily calcium supplement for people aged 65 years or older with a hip or vertebral fracture who are unable to achieve an intake of 1 200 mg/d of calcium from food sources.
Calcium is critical for bone mineralization and strength. The US Recommended Dietary Allowance for calcium is 1200 mg for women aged 50 years or older and men aged 70 years or older [88], although many US adults consume only around half that amount [20]. Studies suggest that obtaining calcium from foods is preferable to taking supplements [20,65], so taking a dietary history before advising supplementation is recommended [20].
Calcium supplements are available in many different forms (e.g. tablets, chews, gums) and often are either calcium carbonate or calcium citrate, although other preparations exist. Whichever form of calcium is used, patients should not take more than 500 to 600 mg at a time in order to maximize absorption [20,88].
Total calcium intake higher than 1 500 mg daily has not been shown to provide additional benefit and potentially could be harmful. Hypercalcemia can contribute to kidney stones, renal insufficiency, and gastrointestinal side effects [20,88]. Whether calcium intake higher than 2 000 mg to 2 500 mg/d increases the risk of myocardial infarction or other cardiovascular events remains somewhat controversial but consumption below that does not appear to raise cardiovascular risk [19,89].
Recommendation 7: Because osteoporosis is a life-long chronic condition, routinely follow and reevaluate people aged 65 years or older with a hip or vertebral fracture who are being treated for osteoporosis. Purposes include:
Reinforcing key messages about osteoporosis and associated fractures;
Identifying any barriers to treatment plan adherence that arise;
Assessing the risk of falling;
Monitoring for adverse treatment effects;
Evaluating the effectiveness of the treatment plan; and
Determining whether any changes in treatment should be made, including whether any anti-osteoporosis pharmacotherapy should be changed or discontinued.
Broken bones are a leading cause of hospitalizations in US women aged 55 years or older, ahead of heart attacks, stroke, and breast cancer [90]. Osteoporosis also affects patients’ health related quality of life on the same scale as diabetes mellitus, heart disease, arthritis, and chronic obstructive pulmonary disease [91,92]. Osteoporosis and broken bones constitute a chronic life-long condition that needs continuing attention and monitoring.
Follow-up with patients aged 65 years or older with hiporvertebral fractures to reinforce key messages about osteoporosis, including answering any questions that patients may have developed since the previous visit. Providing osteoporosis patients with adequate informational support has been shown to be critical to their health-related quality of life [93]. Moreover, failure to meet patients’ educational needs (e.g. medication, self-management, the nature of osteoporosis) has been associated with poor treatment adherence, deterioration of the doctor-patient relationship, and important negative psychosocial consequences [33].
Explore and address any issues with treatment plan adherence that arise [19]. For example, patient adherence with oral bisphosphonates historically has been problematic [94]. Other aspects of treatment plans, such as exercise programs, can also be difficult to accomplish because of changes in health status, transportation issues, lack of facilities, or other problems. Nutritional status, including in adequate calcium, vitamin D, or protein intake, can adversely affect bone health. Treating clinicians need to be aware of these types of barriers and attempt on a regular basis to identify and overcome them.
Routinely assess the risk of falling. That risk can change over time and asking patients whether they have fallen since the last time they were seen takes only a few seconds. Additionally, patients taking bisphosphonates should be reminded and asked about any hip or thigh pain or dental issues (see Recommendation #10).
Various sets of clinical guidelines advise on the best way to monitor patients with fracture. Although they agree on many points, they diverge on other issues, such as the role of following BMD over time in patients taking anti-osteoporosis medications. Those in favor of BMD testing every 1 to 2 years contend that identifying patients who continue to lose bone despite treatment is critical because they may have secondary causes of osteoporosis, need changes to their medication regimens, or be taking their medication incompletely or incorrectly [20,65,95,96]. If BMD is stable, the frequency of BMD measurements can be reduced [65,96]. Those who believe BMD monitoring is not needed assert that change in BMD accounts for only a small fraction (< 20%) of fracture risk reduction on therapy [20]. and that most women will have a reduced risk from medication even if their BMD does not increase [19]. They also maintain that evidence of using serial BMD testing to identify secondary causes of osteoporosis is only anecdotal [65]. The coalition’s clinical recommendations do not take a position on this debate. Recommendation #12 provides additional information about length of pharmacological treatment.
Additional recommendations and rationales
Recommendation 8: Consider referring people aged 65 years or older with a hip or vertebral fracture who have possible or presumed secondary causes of osteoporosis to the appropriate subspecialist for further evaluation and management.
Many postmenopausal women, as well as men, with osteoporosis have factors such as underlying disease or medication use that can contribute to bone weakening [20,64,65,97–102]. Glucocorticoids are probably the most common cause of secondary osteoporosis, but other medications, including proton pump inhibitors, selective serotonin reuptake inhibitors, barbiturates, aromatase inhibitors, loop diuretics, and anticoagulants, among others, have been associated with secondary osteoporosis [97–99]. Medical conditions causing osteoporosis include endocrine disorders (e.g. diabetes mellitus, hyperthyroidism, hyperparathyroidism), kidney and liver disease, malabsorption syndromes, and autoimmune disorders, among others [20,97,99].
Theoretically, identifying and addressing these factors could reduce the risk of secondary fracture [97,100]. There is little agreement on the best approach, however, and evidence of the clinical utility of most testing is not available [92,93]. Clinicians nevertheless need to consider the possibility of secondary causes of osteoporosis, conduct an appropriate history and medical examination, and consider referring patients with possible secondary causes to appropriate subspecialists [5,20,65].
Virtually all published clinical guidelines relating to fractures or osteoporosis include recommendations not to use tobacco and to limit alcohol intake because of these substances’ impact on bone health. Although tobacco use is discouraged in any amount, the recommended upper limits on alcohol intake affecting bone health vary. The consensus recommendation follows CDC definitions of excessive and heavy drinking: for women, 8 or more drinks per week; for men, 15 or more drinks per week [103].
Recommendation 9: Counsel people aged 65 years or older with a hip or vertebral fracture:
Not to smoke or use tobacco;
To limit any alcohol intake to a maximum of 2 drinks a day for men and 1 drink a day for women; and
To exercise regularly (at least three times a week), including weight-bearing, muscle strengthening, and balance and postural exercises, depending on their needs and capabilities, preferably supervised by physical therapists or other qualified professionals.
Clinical guidelines are also united with respect to the importance of recommending exercise for patients with osteoporosis [104] Regular weight-bearing and strength-training exercise can lead to improvements in bone mineral density and also decrease the risk of falls [105–109]. Exercises that focus on balance and trunk muscle strength may be even more effective at preventing falls [20]. Exercise recommendations must be tailored to the individual patient, considering their needs, limitations, and preferences, among other factors, including safety [21,61]. For example, activities that involve forward spine flexion and rotation, side bending, or heavy weights should be approached cautiously because they generate compressive and torsional forces on vertebrae that can result in fracture [20,61].
Although available clinical guidelines are well aligned in terms of types of exercise they advise, they often do not include information about exercise dosage, progression, or contraindications [104]. Thus, physicians should strongly consider referring people aged 65 years or older with hip or vertebral fractures to physical therapists or other qualified professionals for evaluation and exercise plan development.
For patients to make an educated and informed decision about taking anti-osteoporosis medications, they need to understand the risks and benefits of their choices. The prescribing physician needs to take steps to ensure that patients fully understand this material. Guidelines promulgated by the American Association of Clinical Endocrinologists and the American College of Endocrinology [20] discuss osteoporosis risk communication strategies and provide examples of effective presentations, and educational materials are available from other organizations as well.
Recommendation 10: When offering pharmacologic therapy for osteoporosis to people aged 65 years or older with a hip or vertebral fracture, discuss the benefits and risks of therapy, including, among other things:
The risk of osteoporosis-related fractures without pharmacologic therapy; and
For bisphosphonates and denosumab, the risk of atypical femoral fractures (AFFs) and ONJ and how to recognize potential warning signs.
One of the most important aspects of this recommendation is that patients understand the full extent of risks they face without drug treatment of their osteoporosis. The risk of another broken bone is substantially increased – Medicare patients who had a first fracture of the hip or spine had a 20% to 25% chance of a subsequent fracture just within the first year [3] Consequences of second fractures may include loss of independence, the loss of mobility, and increased mortality. Although a full review of how different anti-osteoporosis pharmacologic treatments can reduce these outcomes is beyond the scope of this document, a brief review of evidence concerning bisphosphonates is appropriate because inaccurate perceptions of their benefits and risks are often substantial barriers to appropriate treatment and fracture prevention. Information about a range of available treatments can be found in review articles, such as that by Tu and colleagues [110].
A recent systematic review and meta-analysis examined the effects of bisphosphonates in the specific context of secondary fracture prevention [111]. The analysis included 5 670 participants with osteoporotic fractures from 12 randomized controlled trials with follow-up ranging from 1 month to 3 years. Compared with placebo, bisphosphonates significantly reduced the risk of subsequent fracture (odds ratio [OR] = 0.499) and mortality (OR = 0.662) as well as pain at the fracture site and health-related quality of life. Hip, spine, and wrist fractures all were reduced. These results are consistent with other meta-analyses that have found both clinically important and statistically significant reductions in secondary fractures (hip, vertebral, and nonvertebral) in postmenopausal women taking alendronate [112] or risedronate [113] for at least 1 year.
One of the issues that most concerns patients who have suffered an osteoporotic fracture is the safety of potential therapies and particularly the risk of two specific events: AFFs and ONJ. These conditions have received a great deal of media attention and some survey data suggest that the risks of anti-osteoporosis drugs are overestimated [32]. Because of the importance of this issue to patients, it is important for prescribing physicians to be aware of the evidence and to be sure it is accurately communicated to their patients.
A more detailed case definition is available, but an AFF is a fracture of the femoral shaft or subtrochanteric region that occurs either without any trauma or with low trauma and that has a transverse or short oblique configuration (not including cases of, e.g. pathological fractures due to bone tumors or periprosthetic fractures) [114,115]. AFFs can occur in the general population but are most common in patients who are taking bisphosphonates [116]. There have also been reports of AFF occurring in patients on denosumab and other medications, although many (but not all) of the reported patients also had extensive prior exposure to bisphosphonates [117–121].
It is difficult to be sure of the background incidence of an event as rare as AFF. Moreover, epidemiologic studies describing the incidence of AFF in the general population and in bisphosphonate users vary in the use of radiographic adjudication in their case definitions, as well as study design, treatment and comparator groups, and populations, which adds to the uncertainty. One study of patients in an integrated health care system reported 1) a background incidence in the range of 1 to 2 cases per 100,000 person-years, 2) the risk in patients taking bisphosphonates for 4 to 6 years in the range of 16 cases/100,000 person-years, and 3) the risk in patients taking bisphosphonates for 8 to 10 years in the range of 100 cases/100,000 person-years [122]. An ASBMR task force that reviewed the literature concluded that the incidence of AFF in patients taking bisphosphonates ranges from 3.2 to 50/100,000 person-years, with the incidence increasing with length of treatment [115]. These ranges are roughly consistent and confirm that longer duration of treatment is associated with increased risk of AFF. To place the relative risks in perspective, treatment prevents around 162 osteoporotic fractures for every AFF that occurs [123]. Recommendation #12 provides additional information about potential long-term use of pharmacologic treatments.
Research continues into other risk factors. Metabolic factors, such as impaired response of parathyroid hormone to hypocalcemia, and bone mechanical/geometric factors (e.g. neck-shaft angle) have been suggested as contributing to the risk of AFF [124,125]. Patients who are Asian [114,117], relatively younger (< 65 to 70 years old) [124,126], with higher bone mineral density [127], or have used glucocorticoids for 1 year or more [128] may also have an increased AFF risk. Genetic risk factors may exist as well, although evidence is still developing [129]
It should be noted that in around 70% of the AFF cases reviewed by an expert task force, patients reported a prodrome of thigh or hip pain [115]. Although it is not known whether AFF can be prevented, patients should be told to urgently report thigh or hip pain and should receive radiographic evaluation [21,114,124,125]. Dual-energy X-ray absorptiometry technology is a useful evaluation technique for detecting cortical thickening in the spectrum of AFF [130,131] and some newer densitometers can provide a single energy image of almost the entire femur.
The first reports of ONJ in patients taking bisphosphonates were published in 2003 [132]. The only other anti-osteoporosis drug associated with an increased risk of ONJ is denosumab [133], and the risk appears to be comparable to that associated with bisphosphonates [134]. The exact incidence of ONJ remains unknown but is believed to be 0.001% or less annually in the general population [66,135]. In patients with osteoporosis who are taking usual doses of bisphosphonates, the incidence is estimated to be only slightly higher – somewhere in the range of 0.001% (1/100,000) and 0.01% (1/10,000) [66,123]. More than 90% of the medication related cases occur in patients who have advanced cancer and bone metastases and are taking substantially higher drug doses, more frequently, and often intravenously, to prevent skeletal complications [67,123,135]. Denosumab-related ONJ, for example, has rarely been reported in patients who do not have cancer and who are being treated only for osteoporosis [136]. Similarly, in a systematic review and meta-analysis of cancer patients on bisphosphonates, the risk of ONJ was not significantly increased for patients on oral bisphosphonates – only for those taking the drugs intravenously [137]. In short, the risk of ONJ for patients with osteoporosis taking bisphosphonates or denosumab appears to be only slightly higher than for the general population and the benefit/risk ratio for bisphosphonates remains extremely favourable [2,66].
Risk factors for ONJ can be divided into four main categories: 1. drug-related (type, dose, duration); 2. local (e.g. operative treatment, anatomic factors, concomitant oral disease); 3. demographic and systemic (e.g. age, sex, comorbid conditions); and 4. genetic [138]. The risk factors themselves vary, with one set of factors identified for cancer patients taking high doses of antiresorptives and another set of factors identified for osteoporosis patients taking lower doses. The International Task Force on Osteonecrosis of the Jaw, supported by 14 international societies, names dental extraction and suppuration as the two most important risk factors for osteoporosis patients on bisphosphonates or denosumab [66]. (More information on the risk factors for oncology patients as well as other factors that may increase risk can be found in the International Task Force’s most recent review article) [66]. Although roughly one-third of ONJ cases do not have any clear preceding event, the most common preceding events are local bone infection or trauma [66,67,134,139].
There are steps that clinicians and patients can take to try to reduce the risk of ONJ. First, prescribing clinicians should consider a patient’s oral health before beginning bisphosphonates or denosumab. Additionally, osteoporosis patients can best minimize their risk of ONJ while taking bisphosphonates or denosumab by optimizing and maintaining their dental health. The recommendations are the same as for the general population: maintaining good oral hygiene is of paramount importance and patients should visit their dentist regularly [66,67,138,140]. Minor dental procedures like fillings, inlays, crowns, and scaling can be performed routinely and even procedures like tooth extractions and implant surgery can be performed if needed on osteoporosis patients taking antiresorptives [66,67].
Whether interrupting antiresorptive therapy (“taking a drug holiday”) before undergoing a more extensive dental procedure affects the risk of ONJ is not known [135,140]. Some dental practitioners assert that there are theoretical reasons to suspect that a 2-month drug-free period before undergoing invasive dental treatment may be appropriate for patients with longer (>4 years) exposure histories [138] Nevertheless, the International Task Force, among other professional groups and academics [138,140,141] observes that there is “currently no evidence that interruption of drug therapy in patients requiring dental procedures reduces the risk of ONJ or the progression of the disease” [66].
Patients should be made aware of key signs and symptoms of ONJ, for example jaw or tooth pain, numbness or tingling of the lower lip or chin, loose teeth, signs of infection (swelling, pus exudation, redness, etc.), bad breath, bare bone in the mouth. However, in many cases there is no clear preceding dental event. Although patients should contact their dentists about these signs and symptoms, the clinician who prescribes the bisphosphonate or denosumab is responsible in the first instance for providing the information to the patient.
Finally, more detailed patient management recommendations from the dental perspective are available [66,138], and the published literature includes descriptions of protocols for dental procedures that may reduce the risk of ONJ [142].
Recommendation 11: First-line pharmacologic therapy options for people aged 65 years or older with a hip or vertebral fracture include:
The oral bisphosphonates alendronate and risedronate, which are generally well tolerated, familiar to health care professionals, and available at low cost; and
Intravenous zoledronic acid and subcutaneous denosumab, if oral bisphosphonates pose difficulties.
For patients at high risk of fracture, particularly those with vertebral fractures, anabolic agents may be useful, although consultation with or referral to a specialist would also be appropriate.
Almost all clinical guidelines that address how to reduce the risk of fractures in patients with osteoporosis recommend bisphosphonates as first-line therapies [5,19,20,49,64,65,143]. Alendronate and risedronate are oral bisphosphonates, which function as antiresorptives and have been shown to reduce the risk of hip, vertebral, and nonvertebral fractures in postmenopausal osteoporotic women [5,19,20]. They also are generally well tolerated, easier for patients to self-administer compared with an injection or infusion, and available in generic forms and therefore relatively low cost [5,143]. Although the evidence of their effectiveness in men is less robust, the evidence, focused mostly on bone mineral density endpoints, supports their use in men [21,95]. Oral bisphosphonates are usually taken on a weekly or monthly basis after an overnight fast, and patients must then remain upright and wait at least 30 minutes before ingesting other foods or medicines [20,64]. If patients cannot remain upright for that duration, have esophageal disease that could delay tablet transit, or have problems with gastrointestinal absorption, different medications would likely be more appropriate. All bisphosphonates are known to affect kidney function (regardless of the route of administration) and should be used cautiously, or not at all, in patients with estimated glomerular filtration rates below 30 to 35 mL/min.
Zoledronic acid also has broad antifracture efficacy (reducing the risk of hip, vertebral, and nonvertebral fractures) and is a useful first-line option for patients who have difficulty with oral bisphosphonates. Pretreating patients with acetaminophen 1 or 2 hours before infusion or for a few days after infusion can reduce the risk of a flu-like acute phase reaction (e.g. fever, headache, muscle aches) that otherwise occurs in 30% to 40% of patients during their first infusion [20,64,144–146]. Denosumab is a monoclonal antibody that binds to the cytokine RANKL (receptor activator of nuclear factor kappa-B ligand), thereby inhibiting osteoclasts and functioning primarily as an antiresorptive [147,148]. It also has broad antifracture efficacy, particularly for preventing vertebral fractures, which it reduces by approximately 70% over 3 years [148]. Denosumab is administered by subcutaneous injection every 6 months and is thought to be appropriate for patients with renal insufficiency, although any calcium deficiency, vitamin D deficiency, or secondary hyperparathyroidism should be resolved first and patients with severe insufficiency should be monitored for hypocalcemia [20,64,149,150]. Unlike bisphosphonates, denosumab is not incorporated into the bone matrix and its antiresorptive effects do not continue after treatment is discontinued; rapid transition to another therapy after discontinuation of denosumab is recommended to prevent the risk of fractures from subsequently increasing [64,151].
Depending on individual medical circumstances and other factors, the anabolic agents teriparatide, abaloparatide, and romosozumab may also be useful front-line therapies [19–21,64,74,152–154]. Although favourable fracture healing effects of teriparatide and abaloparatide have been observed in animal models, less is known about their effects in the immediate post-fracture period. In general, anabolic agents have not been recommended as first-line therapies because it is not clear whether they reduce the risk of hip fractures [19–21,95,154], although a recent meta-analysis suggests that they might [155]. They also have substantial costs and are administered by subcutaneous injection – daily for teriparatide and abaloparatide and monthly for romosozumab. They are usually reserved for patients with severe osteoporosis (particularly those with vertebral fractures), for treating glucocorticoid-induced osteoporosis, and for patients in whom alternative therapies are contraindicated [5,21,65,74,95,152]. Use of teriparatide and abaloparatide is generally limited to 2 years because of risk of osteosarcoma (based on rodent studies only, however) and a limited anabolic window, whereas use of romosozumab is limited to 1 year. Because their efficacy falls when stopped, patients should receive an antiresorptive therapy to preserve or perhaps enhance their risk reduction after anabolic drugs are discontinued [20,64,74,152].
It is critical to note this recommendation is general in nature and does not necessarily apply to any specific patient. Choice of therapy should be determined on an individual basis by patients and their physicians. More complete information on the benefits and risks of all potential anti-osteoporosis medications can be found in professional clinical guidelines, the medical literature, and the FDA-approved product labels.
Recommendation 12: The optimal duration of pharmacologic therapy for people aged 65 years and older with a hip or vertebral fracture is not known.
General recommendations on stopping and restarting antiosteoporosis drugs are available to individualize treatment for each patient.
Most published guidelines recommend that the need for therapy with bisphosphonates be reassessed after 3 to 5 years, based on their long half-life in bone and evidence suggesting that the risk of certain rare adverse events may increase with longer duration of treatment.
Stopping denosumab without starting another antiresorptive drug should be avoided because of the possibility of rapid bone loss and increased fracture risk. Similarly, patients stopping anabolic agents also should be placed on an antiresorptive therapy.
The optimal length of pharmacological treatment, particularly for bisphosphonates, is not known [19–21,49,65]. Many of the pivotal trials had durations of a few years, and the small number of trials with longer duration (up to 10 years) provide suggestive but limited data [21,123]. In light of available data and their limitations, periods of bisphosphonate use longer than 3 to 5 years (3 years for intravenous bisphosphonates, 5 years for oral) are generally recommended only for patients at high risk of osteoporotic fracture [19–21,95,123], although there is not universal consensus on this approach [156].
“Drug holidays,” or periods of time when pharmacologic therapy is not given, have been suggested as a clinical approach to address the uncertainty [116], but data are only now emerging on their effects in various populations and results are inconsistent [157]. Experiences of one large cohort of women aged 50 years or older who had used a bisphosphonate suggest that the risk of AFF is reduced by around 40% in the first year of the drug holiday and reduced by around 80% by later years [158]. A drop in risk of AFF, however, would need to be balanced against any increase in the risk of osteoporotic fractures during the holiday and some recent studies indicate that this risk could increase by 30% to 40% within a short time of stopping the medication [159,160]. Other studies, however, have not found an increased risk of osteoporotic fractures in bisphosphonate users who discontinued the drugs for a year or more [161]. Differences in study definitions, patient populations, and methodologies, among other factors, make these results difficult to interpret, but future data may help clarify the expected outcomes.
Unlike bisphosphonates, denosumab is not incorporated into the bone matrix and its antiresorptive effects do not continue after treatment is discontinued; rapid transition to another therapy after discontinuation of denosumab is recommended to prevent the risk of fractures from subsequently increasing [64,151].
Use of the anabolic drugs teriparatide and abaloparatide for more than 2 cumulative years during a patient’s lifetime is not recommended, primarily because of the potential risk of osteosarcoma (based on rodent studies) [86,162] and use of romosozumab is limited to 1 year [74]. Additionally, gains in BMD are lost rapidly when anabolic drugs are stopped, and patients should be continued on an antiresorptive therapy to preserve or perhaps enhance their risk reduction after anabolic drug discontinuation [20,64,74,152].
Recommendation 13: Primary care providers who are treating people aged 65 years and older with a hip or vertebral fracture may want to consider referral to an endocrinologist or osteoporosis specialist for those patients who, while on pharmacotherapy, continue to experience fractures or bone loss without an obvious cause, or who have comorbidities or other factors that complicate management (e.g. hyperparathyroidism, chronic kidney disease).
The decision whether to refer a patient to an endocrinologist or other osteoporosis specialist will usually be made on a case-by-case basis, taking into account factors such as the patient’s specific clinical situation and comorbidities, the physician’s time, resources, and experience, and the availability of an appropriate specialist or FLS program among others. Although less common conditions, like hypercalciuria, hyperparathyroidism, and various malabsorption disorders, may prompt consideration of referral, even some relatively common conditions, like diabetes or chronic kidney disease, can significantly complicate osteoporosis care and may also provide a basis for referral [20]. This recommendation assumes that any issues of therapy adherence have already been addressed.
Conclusion
These consensus recommendations represent the first step toward global efforts to reduce the burden of secondary osteoporotic fractures with their devastating effects on survival, function, and quality of life. The ASBMR Secondary Fracture Prevention Initiative will next launch an action plan including: 1. support, coordination, and expansion of existing secondary fracture prevention registries and data collection; 2. expansion of the use of case management/fracture liaison services; 3. development and dissemination of educational materials for patients and health care professionals; 4. improvement of the diagnosis of and communication about patients with vertebral fractures; 5. exploration of potential uses of reimbursement and financial incentives; 6. continuation of the development of specific quantifiable goals and identification of quality measures; 7. exploration of potential uses of new technologies and staying abreast of the evolution of clinical standards; 8. continuation of the development of pilot programs for preventing secondary fracture for testing in integrated health care delivery systems; 9. building relationships with key organizations that are not coalition members; and 10. continuation of coalition and stakeholder coordination. This set of next steps may be ambitious, but the alternative is to continue along the current path that has neglected to protect patients from a future of suffering.

Disclosures
KA has received consultant fees from Amgen, Eli Lilly, Merck, Renapharma, Sandoz, and UCB; RB has received consultant fees from Novo-Nordisk, UpToDate, McGraw Hill, and Elsevier; CC has received consultant fees from Amgen, Nestle, Servier, Lilly, and UCB; DK has received consultant fees from Solarea Bio; ML has received consultant fees from Amgen, Lilly, UCB Pharma, Radius Health, Meda, Consilient Health, GE-Lunar, and Tromp Medical. KS has received consulting fees from Abbvie, Amgen, Ironwood/AstraZeneca, Bayer, Gilead, Horizon, Kowa, Radius, Roche/Genentech, SOBI, Takeda, and Teijin; SG has received grants from Amgen; MKJ has received grants from Amgen; BC has received grants from Shire/Takeda; DK has received grants from National Dairy Council and Radius Health; KS has received grants from Amgen, Ironwood/AstraZeneca, Horizon, SOBI, and Takeda. MH has received royalties from Elsevier as Editor, Rheumatology 7e and as Editor-in-Chief, Seminars in Arthritis and Rheumatism, and has received stock or stock options from Wolters Kluwer. RB has received nonfinancial support from Amgen, Abbott Laboratories, Abbvie, and Amgen; BC is a Data Monitoring Board Member for Bristol Myers-Squibb; MH has received personal fees and nonfinancial support from Eli Lilly, Novartis Pharma AG, Pfizer, and Wolters Kluwer as a contributor to UpToDate; KS is Secretary of the American College of Rheumatology.
Acknowledgments
Authors’ roles: Literature review: RC. Drafting manuscript: RC, SK, DK, and AE. Revising manuscript content: GA, RA, KEA, IA, KCA, RB, WB, EC, KC-N, BC, KC, RC, CC, CJC, DD, MD, TE, AE, MF, SG, PH, SH, MH. MJ. KJ, AK, SK, DK, TK, TFK, JK, MK, CL, GL, LM, AM, SM, NM, NN, TO, JP, SR, CR, KS, ET, LT, and HT. Approving final version of manuscript: GA, RA, KEA, IA, KCA, RB, WB, EC, KC-N, BC, KC, RC, CC, CJC, DD, MD, TE, AE, MF, SG, PH, SH, MH. MJ. KJ, AK, SK, DK, TK, TFK, JK, MK, CL, GL, LM, AM, SM, NM, NN, TO, JP, SR, CR, KS, ET, LT, and HT.
Non-author contributors: Lyndon Joseph, PhD, National Institute on Aging, participated in developing the clinical recommendations and reviewing manuscript content. Emily A Kuhl, PhD, Right Brain/Left Brain, LLC, participated in technical editing of the manuscript. Dexter Waters, MSPH, Center for Medical Technology Policy, participated in the literature review.
Douglas P Kiel, MD | kiel@hsl.harvard.edu | www.hms.harvard.edu
Received in original form August 14, 2019; revised form September 8, 2019; accepted September 11, 2019. Accepted manuscript online September 20, 2019. Address correspondence to: Douglas P Kiel, MD, Harvard Medical School, Musculoskeletal Research Center, Marcus Institute for Aging Research, Hebrew SeniorLife, 1 200 Centre Street, Boston, MA 02131, USA. E-mail: kiel@hsl.harvard.edu
Journal of Bone and Mineral Research, Vol. 35, No. 1, January 2020, pp 36–52.
Available at DOI: <http://DOI: 10.1002/jbmr.3877>.
©2019 American Society for Bone and Mineral Research
The article is reprinted with the permission of the first author and the publisher | Článek je přetištěn se souhlasem prvního autora a vydavatele
Received in original form August 14, 2019; revised form September 8, 2019; accepted September 11, 2019. Accepted manuscript online September 20, 2019. Address correspondence to: Douglas P Kiel, MD, Harvard Medical School, Musculoskeletal Research Center, Marcus Institute for Aging Research, Hebrew SeniorLife, 1 200 Centre Street, Boston, MA 02131, USA. E-mail: kiel@hsl.harvard.edu
Journal of Bone and Mineral Research, Vol. 35, No. 1, January 2020, pp 36–52.
Available at DOI: <http://DOI: 10.1002/jbmr.3877>.
©2019 American Society for Bone and Mineral Research
The article is reprinted with the permission of the first author and the publisher | Článek je přetištěn se souhlasem prvního autora a vydavatele
Zdroje
Khosla S, Shane E. A crisis in the treatment of osteoporosis. J Bone Miner Res 2016; 31(8): 1485–7.
Khosla S, Cauley JA, Compston J et al. Addressing the crisis in the treatment of osteoporosis: a path forward. J Bone Miner Res 2017; 32(3): 424–30.
Weaver J, Sajjan S, Lewiecki EM, Harris ST, Marvos P. Prevalence and cost of subsequent fractures among U.S. patients with an incident fracture. J Manag Care Spec Pharm 2017; 23(4): 461–71.
Eisman JA, Bogoch ER, Dell R et al. Making the first fracture the last fracture: ASBMR task force report on secondary fracture prevention. J Bone Miner Res 2012; 27(10): 2039–46.
Lems WF, Dreinhofer KE, Bischoff-Ferrari H et al. EULAR/EFORT recommendations for management of patients older than 50 years with a fragility fracture and prevention of subsequent fractures. Ann Rheum Dis 2017; 76(5): 802–10.
Wu CH, Tu ST, Chang YF et al. Fracture liaison services improve outcomes of patients with osteoporosis-related fractures: a systematic literature review and meta-analysis. Bone 2018; 111: 92–100.
Wu CH, Chen CH, Chen PH et al. Identifying characteristics of an effective fracture liaison service: systematic literature review. Osteoporos Int 2018; 29(5): 1023–47.
Wu CH, Kao IJ, Hung WC et al. Economic impact and cost effectiveness of fracture liaison services: a systematic review of the literature. Osteoporos Int 2018; 29(6): 1227–42.
Dunn P, Webb D, Olenginski TP. Geisinger high-risk osteoporosis clinic (HiROC): 2013–2015 FLS performance analysis. Osteoporos Int 2018; 29(2): 451–7.
Olenginski TP, Maloney-Saxon G, Matzko CK et al. High-risk osteoporosis clinic (HiROC): improving osteoporosis and post-fracture care with an organized, programmatic approach. Osteoporos Int 2015; 26(2): 801–10.
Greenspan SL, Singer A, Vujevich K et al. Implementing a fracture liaison service open model of care utilizing a cloud-based tool. Osteoporos Int 2018; 29(4): 953–60.
Stephenson S, National Osteoporosis Society. Establishing and implementing a fracture liaison service. Ann Rheum Dis 2017; 76 (Suppl 2): 30 (SPO 118).
(FLS-DB) FLSD. Fracture liaison service database: commissioner’s report 2018 [Internet]. 2018. Available at WWW: <https://www.rcplondon. ac.uk/projects/outputs/fracture-liaison-service-databasecommissioners-report-2018>.
American Orthopaedic Association. What is own the bone? [Internet]. Available at WWW: <https://www.ownthebone.org/OTB/About/What_Is_Own_the_Bone.aspx>. Accessed October 29, 2018.
National Osteoporosis Foundation. Fracture Liaison Service (FLS) Certificate Program [Internet]. Available at WWW: <https://www.cme.nof. org/Training.aspx>. Accessed March 5, 2019.
International Osteoporosis Foundation. Capture the fracture with new resources and increased outreach [Internet]. 2017. Available at WWW: <https://www.iofbonehealth.org/about-us/annual-report/capturefracture-new-resources-and-increased-outreach>. Accessed October 29, 2018.
Mace H, NHS England. A national approach to reducing fragility fractures [Internet]. 2016. Available at WWW: <https://www.england.nhs.uk/blog/henry-mace/>.
National Bone Health Alliance. Fracture prevention central. 2015. Available at WWW: <http://www.nbha.org/fpc>. Accessed October 29, 2018.
Qaseem A, Forciea MA, McLean RM, Denberg TD. Clinical guidelines Committee of the American College of Physicians. Treatment of low bone density or osteoporosis to prevent fractures in men and women: a clinical practice guideline update from the American College of Physicians. Ann Intern Med 2017; 166(11): 818–39.
Camacho PM, Petak SM, Binkley N et al. American Association of Clinical Endocrinologists and American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis – 2016 – executive summary. Endocr Pract 2016; 22(9): 1111–8.
Compston J, Cooper A, Cooper C et al. UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos 2017; 12(1): 43.
Ross PD, Davis JW, Epstein RS, Wasnich RD. Pre-existing fractures and bone mass predict vertebral fracture incidence in women. Ann Intern Med 1991; 114(11): 919–23.
Kanis JA, Johnell O, De Laet C et al. A meta-analysis of previous fracture and subsequent fracture risk. Bone 2004; 35(2): 375–82.
Cauley JA, Hochberg MC, Lui LY et al. Long-term risk of incident vertebral fractures. JAMA 2007; 298(23): 2761–7.
Tajeu GS, Delzell E, Smith W et al. Death, debility, and destitution following hip fracture. J Gerontol A Biol Sci Med Sci 2014; 69(3): 346–53.
Peeters CM, Visser E, Van de Ree CL, Gosens T, Den Oudsten BL, De Vries J. Quality of life after hip fracture in the elderly: a systematic literature review. Injury 2016; 47(7): 1369–82.
Kim SM, Moon YW, Lim SJ et al. Prediction of survival, second fracture, and functional recovery following the first hip fracture surgery in elderly patients. Bone 2012; 50(6): 1343–50.
Hansson S, Rolfson O, Akesson K, Nemes S, Leonardsson O, Rogmark C. Complications and patient-reported outcome after hip fracture. A consecutive annual cohort study of 664 patients. Injury 2015; 46(11): 2206–11.
Dailiana Z, Papakostidou I, Varitimidis S, Michalitsis S, Veloni A, Malizos K. Surgical treatment of hip fractures: factors influencing mortality. Hippokratia 2013; 17(3): 252–7.
Mariconda M, Costa GG, Cerbasi S, et al. Factors predicting mobility and the change in activities of daily living after hip fracture: a 1-year prospective cohort study. J Orthop Trauma 2016; 30(2): 71–7.
BueckingB, EschbachD, KnobeM et al. Predictors of noninstitutionalized survival 1 year after hip fracture: a prospective observational study to develop the Marburg rehabilitation tool for hip fractures (MaRTHi). Medicine (Baltimore) 2017; 96(37): e7820.
BoudreauDM, YuO, BalasubramanianA et al. A survey of women’s awareness of and reasons for lack of post fracture osteoporotic care. J Am Geriatr Soc 2017; 65(8): 1829–35.
Raybould G, Babatunde O, Evans AL, Jordan JL, Paskins Z. Expressed information needs of patients with osteoporosis and/or fragility fractures: a systematic review. Arch Osteoporos 2018; 13(1): 55.
Adams J CE, Clunie G et al. Clinical guidance for the effective identification of vertebral fractures [Internet]. 2017. Available at WWW: <https://theros.org.uk/media/100017/vertebral-fracture-guidelines.pdf>. Accessed September 4, 2019.
Majumdar SR, Kim N, Colman I et al. Incidental vertebral fractures discovered with chest radiography in the emergency department: prevalence, recognition, and osteoporosis management in a cohort of elderly patients. Arch Intern Med 2005; 165(8): 905–9.
Bartalena T, Rinaldi MF, Modolon C et al. Incidental vertebral compression fractures in imaging studies: lessons not learned by radiologists. World J Radiol 2010; 2(10): 399–404.
Li Y, Yan L, Cai S, Wang P, Zhuang H, Yu H. The prevalence and under-diagnosis of vertebral fractures on chest radiograph. BMC Musculoskelet Disord 2018; 19(1): 235.
Mitchell RM, Jewell P, Javaid MK, McKean D, Ostlere SJ. Reporting of vertebral fragility fractures: can radiologists help reduce the number of hip fractures? Arch Osteoporos 2017; 12(1): 71.
van Geel TA, van Helden S, Geusens PP, Winkens B, Dinant GJ. Clinical subsequent fractures cluster in time after first fractures. Ann Rheum Dis 2009; 68(1): 99–102.
Ensrud KE. Epidemiology of fracture risk with advancing age. J Gerontol A Biol Sci Med Sci 2013; 68(10): 1236–42.
Gillespie LD, Robertson MC, Gillespie WJ et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2012; 9: CD007146.
Youm T, Koval KJ, Kummer FJ, Zuckerman JD. Do all hip fractures result from a fall? Am J Orthop (Belle Mead NJ) 1999; 28(3): 190–4.
Morrison A, Fan T, Sen SS, Weisenfluh L. Epidemiology of falls and osteoporotic fractures: a systematic review. Clinicoecon Outcomes Res 2013; 5: 9–18.
Centers for Disease Control and Prevention, Division of Unintentional Injury Prevention. Hip fractures among older adults [Internet]. 2016. Available at WWW: <https://www.cdc.gov/homeandrecreationalsafety/ falls/adulthipfx.html>. Accessed October 31, 2018.
Mayo Clinic. Hip fracture – symptoms and causes [Internet]. 2019. Available at WWW: <https://www.mayoclinic.org/diseases-conditions/hipfracture/symptoms-causes/syc-20373468>. Accessed June 26, 2019.
Johns Hopkins Medicine. Hip fractures: five powerful steps to prevention [Internet]. 2019. Available at WWW: <https://www.hopkinsmedicine.org/health/wellness-and-prevention/hip-fractures-five-powerfulsteps-to-prevention>. Accessed June 26, 2019.
Slear T. Prevent a hip fracture – avoid falls osteoporosis [Internet]. 2011. Available at WWW: <http://www.aarp.org/health/conditions-treatments/info-10–2011/prevent-hip-fracture.html>. Accessed June 26, 2019.
US Preventive Services Task Force, Grossman DC, Curry SJ et al. Interventions to prevent falls in community-dwelling older adults: US Preventive Services Task Force recommendation statement. JAMA 2018; 319(16): 1696–704.
Kanis JA, Cooper C, Rizzoli R et al. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 2019; 30(1): 3–44.
de Vries M, Seppala LJ, Daams JG et al. Fall-risk-increasing drugs: a systematic review and meta-analysis: I. cardiovascular drugs. J Am Med Dir Assoc 2018; 19(4): 371 e1–9.
Seppala LJ, Wermelink A, deVries M et al. Fall-risk-increasingdrugs: a systematic review and meta-analysis: II. Psychotropics. J Am Med Dir Assoc 2018; 19(4): 371 e11–7.
Seppala LJ, van der Velde N, Masud T et al. EuGMS task and finish group on fall-risk-increasing drugs (FRIDs): position on knowledge dissemination, management, and future research. Drugs Aging 2019; 36(4): 299–307.
Chiba Y, Kimbara Y, Kodera R et al. Risk factors associated with falls in elderly patients with type 2 diabetes. J Diabetes Complications 2015; 29(7): 898–902.
Nyman SR, Ballinger C, Phillips JE, Newton R. Characteristics of outdoor falls among older people: a qualitative study. BMC Geriatr 2013; 13: 125.
Gazibara T, Kurtagic I, Kisic-Tepavcevic D et al. Falls, risk factors and fear of falling among persons older than 65 years of age. Psychogeriatrics 2017; 17(4): 215–23.
Stevens JA. ACDC compendium of effective fall interventions: what works for community-dwelling older adults. 3rd ed. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2015.
Panelon Prevention of Falls in Older Persons, AGS/BGS. Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc 2011; 59(1): 148–57.
JohnstonYA, Bergen G, Bauer M et al. Implementation of the Stopping Elderly Accidents, Deaths, and Injuries Initiative in primary care: an outcome evaluation. Gerontologist. 2018 Sep 20. Available at DOI: <http://dx.doi.org/10.1093/geront/gny101>.
Centers for Disease Control and Prevention, Division of Unintentional Injury Prevention. Make STEADI part of your medical practice [Internet]. 2017. Available at WWW: <https://www.cdc.gov/steadi/index. html>. Accessed October 31, 2018.
National Institute of Arthritis and Musculoskeletal and Skin Diseases. Once is enough: a guide to preventing future fractures [Internet]. 2015. Available at WWW: <https://www.bones.nih.gov/health-info/ bone/osteoporosis/fracture>. Accessed October 31, 2018.
Kerr C, Bottomley C, Shingler S et al. The importance of physical function to people with osteoporosis. Osteoporos Int 2017; 28(5): 1597–607.
Nevitt MC, Ross PD, Palermo L, Musliner T, Genant HK, Thompson DE. Association of prevalent vertebral fractures, bone density, and alendronate treatment with incident vertebral fractures: effect of number and spinal location of fractures. The Fracture Intervention Trial Research Group. Bone 1999; 25(5): 613–9.
Kanis JA, Harvey NC, Johansson H, Oden A, Leslie WD, McCloskey EV. FRAX and fracture prediction without bone mineral density. Climacteric 2015; 18(Suppl 2): 2–9.
Cosman F, de Beur SJ, LeBoff MS et al. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 2014; 25(10): 2359–81.
Watts NB, Adler RA, Bilezikian JP et al. Osteoporosis in men: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 2012; 97(6): 1802–22.
Khan AA, Morrison A, Kendler DL et al. Case-based review of osteonecrosis of the jaw (ONJ) and application of the international recommendations for management from the International Task Force on ONJ. J Clin Densitom 2017; 20(1): 8–24.
Otto S, Pautke C, Vanden Wyngaert T, Niepe lD, Schiodt M. Medication-related osteonecrosis of the jaw: prevention, diagnosis and management in patients with cancer and bone metastases. Cancer Treat Rev 2018; 69: 177–87.
Khan AA, Sandor GK, Dore E et al. Canadian consensus practice guidelines for bisphosphonate associated osteonecrosis of the jaw. J Rheumatol 2008; 35(7): 1391–7.
Vannucci L, Brandi ML. Healing of the bone with anti-fracture drugs. Expert Opin Pharmacother 2016; 17(17): 2267–72.
Xue D, Li F, Chen G, Yan S, Pan Z. Do bisphosphonates affect bone healing? A meta-analysis of randomized controlled trials. J Orthop Surg Res 2014; 9: 45.
Hak DJ. The biology of fracture healing in osteoporosis and in the presence of anti-osteoporotic drugs. Injury 2018; 49(8): 1461–5.
Colon-Emeric C, Nordsletten L, Olson S et al. Association between timing of zoledronic acid infusion and hip fracture healing. Osteoporos Int 2011; 22(8): 2329–36.
Body JJ, von Moos R, Niepel D, Tombal B. Hypocalcaemia in patients with prostate cancer treated with a bisphosphonate or denosumab: prevention supports treatment completion. BMC Urol 2018; 18(1): 81.
Amgen Inc. EVENITY full prescribing information [Internet]. 2019. Available at WWW: <https://www.evenityhcp.com/gclid=CjwKCAjw0tHoBRBhEiwAvP1GFeK5AYoqD210IPZFIFfRUIDT4NLsdzly1cEgjPy1BQCQTOxsBPh-hoCKsAQAvD_BwE&gclsrc=aw.ds>. Accessed June 27, 2018.
Wang LH, Xu DJ, Wei XJ, Chang HT, Xu GH. Electrolyte disorders and aging: risk factors for delirium in patients undergoing orthopedic surgeries. BMC Psychiatry 2016; 16(1): 418.
Novartis. Highlights for prescribing information for reclast [Internet]. Available at WWW: <https://www.pharma.us.novartis.com/sites/www.pharma.us.novartis.com/files/reclast.pdf?>. Accessed December 6, 2018.
Amgen Inc. Highlights and full prescribing information for Prolia® (denosumab) [Internet]. Available at WWW: <https://www.pi.amgen.com/~/media/amgen/repositorysites/pi-amgen-com/prolia/prolia_pi.pdf>. Accessed December 6, 2018.
Gai P, Sun H, Sui L, Wang G. Hypocalcaemia after total knee arthroplasty and its clinical significance. Anticancer Res 2016; 36(3): 1309–11.
Binkley N, Coursin D, Krueger D et al. Surgery alters parameters of vitamin D status and other laboratory results. Osteoporos Int 2017; 28(3): 1013–20.
Lepage R, Legare G, Racicot C et al. Hypocalcemia induced during major and minor abdominal surgery in humans. J Clin Endocrinol Metab 1999; 84(8): 2654–8.
Lyles KW, Colon-Emeric CS, Magaziner JS et al. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med 2007; 357(18):1799–809.
Reid IR, Gamble GD, Mesenbrink P, Lakatos P, Black DM. Characterization of and risk factors for the acute-phase response after zoledronic acid. J Clin Endocrinol Metab 2010; 95(9): 4380–7.
Hamdy RC. Zoledronic acid: clinical utility and patient considerations in osteoporosis and low bone mass. Drug Des Devel Ther 2010; 4: 321–35.
Crotti C, Watts NB, De Santis M et al. Acute phase reactions after zoledronic acid infusion: protective role of 25-hydroxyvitamin D and previous oral bisphosphonate therapy. Endocr Pract 2018; 24(5): 405–10.
Eli Lilly and Company. FORTEO – teriparatide injection, solution [Internet]. 2002. Available at WWW: <http://uspl.lilly.com/forteo/forteo. html>. Accessed November 13, 2018.
Radius Health Inc. TYMLOS (abaloparatide) injection HCP: for postmenopausal women with a recent osteoporotic fracture: help reduce the risk of fractures [Internet]. 2018. Available at WWW: <https://www.tymloshcp.com/gclid=CjwKCAjwio3dBRAqEiwAHWsNVQBj1_9BzeEKy7X1IKQqAJFb9Xwj_592nLGdHDw_4Sx_rMemgHFmoRoCXLYQAvD_BwE>. Accessed September 20, 2018.
National Institutes of Health. Vitamin D – fact sheet for health professionals [Internet]. 2018. Available at WWW: <https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/>. Accessed September 16, 2018.
National Institutes of Health. Calcium – fact sheet for health professionals [Internet]. 2018. Available at WWW: <https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional/>. Accessed November 6, 2018.
Kopecky SL, Bauer DC, Gulati M et al. Lack of evidence linking calcium with or without vitamin D supplementation to cardiovascular disease in generally healthy adults: a clinical guideline from the National Osteoporosis Foundation and the American Society for Preventive Cardiology. Ann Intern Med 2016; 165 (12): 867–8.
Singer A, Exuzides A, Spangler L et al. Burden of illness for osteoporotic fractures compared with other serious diseases among postmenopausal women in the United States. Mayo Clin Proc 2015; 90(1): 53–62.
Sawka AM, Thabane L, Papaioannou A et al. Health-related quality of life measurements in elderly Canadians with osteoporosis compared to other chronic medical conditions: a population-based study from the Canadian Multicentre Osteoporosis Study (CaMos). Osteoporos Int 2005; 16(12): 1836–40.
Voko Z, Gaspar K, Inotai A et al. Osteoporotic fractures may impair life as much as the complications of diabetes. J Eval Clin Pract 2017; 23(6): 1375–80.
Huang CY, Liao LC, Tong KM et al. Mediating effects on health related quality of life in adults with osteoporosis: a structural equation modeling. Osteoporos Int 2015; 26(3): 875–83.
Black DM, Rosen CJ. Clinical practice. Postmenopausal osteoporosis. N Engl J Med 2016; 374(3): 254–62.
Lagari V, Gavcovich T, Levis S. The good and the bad about the 2017 American College of Physicians Osteoporosis Guidelines. Clin Ther 2018; 40(1): 168–76.
International Society for Clinical Densitometry. 2019 ISCD official positions – adult – International Society for Clinical Densitometry (ISCD) [Internet]. 2019. Available at WWW: <https://www.iscd.org/officialpositions/2015-iscd-official-positions-adult/>. Accessed November 13, 2018.
Mirza F, Canalis E. Management of endocrine disease: secondary osteoporosis: pathophysiology and management. Eur J Endocrinol 2015; 173(3): R131–51.
Skjodt MK, Ostadahmadli Y, Abrahamsen B. Longterm time trend sinuse of medications associated with risk of developing osteoporosis: nationwide data for Denmark from 1999 to 2016. Bone 2019; 120: 94–100.
International Osteoporosis Foundation. Secondary osteoporosis [Internet]. 2017. Available at WWW: <https://www.iofbonehealth.org/secondary-osteoporosis>. Accessed September 16, 2018.
Fink HA, Litwack-Harrison S, Taylor BC et al. Clinical utility of routine laboratory testing to identify possible secondary causes in older men with osteoporosis: the Osteoporotic Fractures in Men (MrOS) Study. Osteoporos Int 2016; 27(1): 331–8.
Ryan CS, Petkov VI, Adler RA. Osteoporosis in men: the value of laboratory testing. Osteoporos Int 2011; 22(6): 1845–53.
Tannenbaum C, Clark J, Schwartzman K et al. Yield of laboratory testing to identify secondary contributors to osteoporosis in otherwise healthy women. J Clin Endocrinol Metab 2002; 87(10): 4431–7.
Division of Population Health, Centers for Disease Control and Prevention. CDC – fact sheets – alcohol use and your health [Internet]. 2018. Available at WWW: <https://www.cdc.gov/alcohol/fact-sheets/ alcohol-use.htm>. Accessed November 28, 2018.
Armstrong JJ, Rodrigues IB, Wasiuta T, MacDermid JC. Quality assessment of osteoporosis clinical practice guidelines for physical activity and safe movement: an AGREE II appraisal. Arch Osteoporos 2016; 11: 6.
Howe TE, Shea B, Dawson LJ et al. Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Syst Rev 2011; 7: CD000333.
Giangregorio LM, Macintyre NJ, Thabane L, Skidmore CJ, Papaioannou A. Exercise for improving outcomes after osteoporotic vertebral fracture. Cochrane Database Syst Rev 2013; 1: CD008618.
Gomez-Cabello A, Ara I, Gonzalez-Aguero A, Casajus JA, Vicente Rodriguez G. Effects of training on bone mass in older adults: a systematic review. Sports Med 2012; 42(4): 301–25.
Zehnacker CH, Bemis-Dougherty A. Effect of weighted exercises on bone mineral density in postmenopausal women. A systematic review. J Geriatr Phys Ther 2007; 30(2): 79–88.
Bolam KA, van Uffelen JG, Taaffe DR. The effect of physical exercise on bone density in middle-aged and older men: a systematic review. Osteoporos Int 2013; 24(11): 2749–62.
Tu KN, Lie JD, Wan CKV, et al. Osteoporosis: a review of treatment options. P T 2018; 43(2): 92–104.
Lee SY, Jung SH, Lee SU, Ha YC, Lim JY. Can bisphosphonates prevent recurrent fragility fractures? A systematic review and metaanalysis of randomized controlled trials. J Am Med Dir Assoc 2018; 19(5): 384–90 e1.
Wells GA, Cranney A, Peterson J et al. Alendronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev 2008; 1: CD001155.
Wells G, Cranney A, Peterson J et al. Risedronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev 2008; 1:CD004523.
Al-Ashqar M, Panteli M, Chakrabarty G, Giannoudis PV. Atypical fractures: an issue of concern or a myth? Injury 2018; 49(3): 649–55.
Shane E, Burr D, Abrahamsen B et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 2014; 29(1): 1–23.
Black DM, Abrahamsen B, Bouxsein ML, Einhorn T, Napoli N. Atypical femur fractures: review of epidemiology, relationship to bisphosphonates, prevention, and clinical management. Endocr Rev 2019; 40(2): 333–68.
Starr J, Tay YKD, Shane E. Current understanding of epidemiology, pathophysiology, and management of atypical femur fractures. Curr Osteoporos Rep 2018; 16(4): 519–29.
Khow KS, Yong TY. Atypical femoral fracture in a patient treated with denosumab. J Bone Miner Metab 2015; 33(3): 355–8.
Ramchand SK, Chiang CY, Zebaze RM, Seeman E. Recurrence of bilateral atypical femoral fractures associated with the sequential use of teriparatide and denosumab: a case report. Osteoporos Int 2016; 27(2): 821–5.
Selga J, Nunez JH, Minguell J, Lalanza M, Garrido M. Simultaneous bilateral atypical femoral fracture in a patient receiving denosumab: case report and literature review. Osteoporos Int 2016; 27(2): 827–32.
Papapoulos S, Lippuner K, Roux C et al. The effect of 8 or 5 years of denosumab treatment in postmenopausal women with osteoporosis: results from the FREEDOM extension study. Osteoporos Int 2015; 26(12): 2773–83.
Dell RM, Adams AL, Greene DF et al. Incidence of atypical nontraumatic diaphyseal fractures of the femur. J Bone Miner Res 2012; 27(12): 2544–50.
Adler RA, El-Hajj Fuleihan G, Bauer DC et al. Managing osteoporosis in patients on long-term bisphosphonal tetreatment: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 2016; 31(1): 16–35.
Kharwadkar N, Mayne B, Lawrence JE, Khanduja V. Bisphosphonates and atypical subtrochanteric fractures of the femur. Bone Joint Res 2017; 6(3): 144–53.
Taormina DP, Marcano AI, Karia R, Egol KA, Tejwani NC. Symptomatic atypical femoral fractures ar erelated to under lying hip geometry. Bone 2014; 63: 1–6.
KhowK S, Shibu P, YuS C, Chehade MJ, Visvanathan R. Epidemiology and postoperative outcomes of atypical femoral fractures in older adults: a systematic review. J Nutr Health Aging 2017; 21(1): 83–91.
Black DM, Li BH, Ryan DS, Dell RM, Adams AL. Bisphosphonate use and risk of AFF varies by pre-treatment BMD level: results from the Southern California Osteoporosis Cohort Study (SOCS). 2018 American Society for Bone and Mineral Research Annual Meeting; September 28–October 1, 2018; Montreal, Canada.
Koh JH, Myong JP, Yoo J et al. Predisposing factors associated with atypical femur fracture among postmenopausal Korean women receiving bisphosphonate therapy: 8 years’ experience in a single center. Osteoporos Int 2017; 28(11): 3251–9.
Nguyen HH, van de Laarschot DM, Verkerk A, Milat F, Zillikens MC, Ebeling PR. Genetic risk factors for atypical femoral fractures (AFFs): a systematic review. JBMR Plus 2018; 2(1): 1–11.
van de Laarschot DM, Smits AA, Buitendijk SK, Stegenga MT, Zillikens MC. Screening for atypical femur fractures using extended femur scans by DXA. J Bone Miner Res 2017; 32(8): 1632–9.
Kim S, Yang KH, Lim H, et al. Detection of prefracture hip lesions in atypical subtrochanteric fracture with dual-energy x-ray absorptiometry images. Radiology 2014; 270(2): 487–95.
Marx RE. Pamidronate (Aredia) and zoledronate (Zometa) induced a vascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg 2003; 61(9): 1115–7.
Center for Scientific Information, ADA. Osteoporosis medications and medication-related osteonecrosis of the jaw [Internet]. 2018. Available at WWW: <https://www.ada.org/en/member-center/oral-healthtopics/osteoporosis-medications>. Accessed November 7, 2018.
Aljohani S, Gaudin R, Weiser J et al. Osteonecrosis of the jaw in patients treated with denosumab: a multicenter case series. J Craniomaxillofac Surg 2018; 46(9): 1515–25.
Abed HH, Al-Sahafi EN. The role of dental care providers in the management of patients prescribed bisphosphonates: brief clinical guidance. Gen Dent 2018; 66(3): 18–24.
Voss PJ, Steybe D, Poxleitner P, et al. Osteonecrosis of the jaw in patients transitioning from bisphosphonates to denosumab treatment for osteoporosis. Odontology 2018; 106(4): 469–80.
Lee SH, Chan RC, Chang SS et al. Use of bisphosphonates and the risk of osteonecrosis among cancer patients: a systemic review and meta-analysis of the observational studies. Support Care Cancer 2014; 22(2): 553–60.
Ruggiero SL, Dodson TB, Fantasia J, et al. American Association of Oral and Maxillofacial Surgeons position paper on medication related osteonecrosis of the jaw – 2014 update. J Oral Maxillofac Surg 2014; 72(10): 1938–56.
Chiu WY, Yang WS, Chien JY, Lee JJ, Tsai KS. The influence of alendronate and tooth extraction on the incidence of osteonecrosis of the jaw among osteoporotic subjects. PLoS One 2018; 13(4): e0196419.
Aparecida Cariolatto F, Carelli J, de Campos MT, Pietrobon R, Rodrigues C, Bonilauri Ferreira AP. Recommendations for the prevention of bisphosphonate-related osteonecrosis of the jaw: a systematic review. J Evid Based Dent Pract 2018; 18(2): 142–52.
Diniz-Freitas M, Limeres J. Prevention of medication-related osteonecrosis of the jaws secondary to tooth extractions. A systematic review. Med Oral Patol Oral Cir Bucal 2016; 21(2): e250–9.
Shudo A, Kishimoto H, Takaoka K, Noguchi K. Long-term oral bisphosphonates delay healing after tooth extraction: a single institutional prospective study. Osteoporos Int 2018; 29(10): 2315–21.
Dell R, Greene D. A proposal for an atypical femur fracture treatment and prevention clinical practice guideline. Osteoporos Int 2018; 29 (6): 1277–83.
Black DM, Delmas PD, Eastell R et al. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Eng J Med 2007; 356(18): 1809–22.
Nakamura T, Fukunaga M, Nakano T et al. Efficacy and safety of once-yearly zoledronicacid in Japanese patients with primary osteoporosis: two-year results from a randomized placebo-controlled double-blind study (ZOledroNate treatment in efficacy to osteoporosis; ZONE study). Osteoporos Int 2017; 28(1): 389–98.
Okimoto NSA, Matsumoto H et al. Design of a multicenter, randomized, open label, parallel group study to evaluate the efficacy of loxoprofen on acute-phase reactions in Japanese primary osteoporosis patients treated with zoledronic acid. J Clin Trials 2017; 7(6): 1000336.
Hanley DA, Adachi JD, Bell A, Brown V. Denosumab: mechanism of action and clinical outcomes. Int J Clin Pract 2012; 66(12): 1139–46.
Cummings SR, SanMartin J, McClung MR et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med 2009; 361(8): 756–65.
Nitta K, Yajima A, Tsuchiya K. Management of osteoporosis in chronic kidney disease. Intern Med 2017; 56(24): 3271–6.
Wilson LM, Rebholz CM, Jirru E et al. Benefits and harms of osteoporosis medications in patients with chronic kidney disease: a systematic review and meta-analysis. Ann Intern Med 2017; 166(9): 649–58.
Cummings SR, Ferrari S, Eastell R et al. Vertebral fractures after discontinuation of denosumab: a post hoc analysis of the randomized placebo-controlled FREEDOM trial and its extension. J Bone Miner Res 2018; 33(2): 190–8.
Haas AV, LeBoff MS. Osteoanabolic agents for osteoporosis. J Endocr Soc 2018; 2(8): 922–32.
KanisJ A, Cooper C, Rizzoli R, Reginster JY. Review of the guideline of the American College of Physicians on the treatment of osteoporosis. Osteoporos Int 2018; 29(7): 1505–10.
FDA Office of New Drugs, FDA Office of Surveillance and Epidemiology, FDA Office of Clinical Pharmacology. FDA briefing document: meeting of the Bone, Reproductive and Urologic Drugs Advisory Committee. 2019. Available at WWW: <https://www.fda.gov/media/ 121257/download>. Accessed June 27, 2019.
Diez-Perez A, Marin F, Eriksen EF, Kendler DL, Krege JH, Delgado Rodriguez M. Effects of teriparatide on hip and upper limb fractures in patients with osteoporosis: a systematic review and meta-analysis. Bone 2019; 120: 1–8.
Ott SM. Long-term bisphosphonates: primum non nocere. Menopause 2016; 23(11): 1159–61.
Fink HA, MacDonald R, Forte ML et al. Long-term drug therapy and drug discontinuations and holidays for osteoporosis fracture prevention: a systematic review. Ann Intern Med 2019; 171(1): 37–50.
Adams AL, Ryan DS, Geiger EJ, Dell RM, Black DM. Do drug holidays reduce atypical femur fracture risk? Results from the Southern California Cohort Study (SOCS). 2018 American Society for Bone and Mineral Research Annual Meeting; 2018; Montreal, Canada.
Mignot MA, Taisne N, Legroux I, Cortet B, PaccouJ. Bisphosphonate drug holidays in postmenopausal osteoporosis: effect on clinical fracture risk. Osteoporos Int 2017; 28(12): 3431–8.
Curtis JR, Li Z et al. The impact of the duration of bisphosphonate drug holidays on hip fracture rates. 2017 ACR/ARHP Annual Meeting; 2018; San Diego, CA, USA.
Adams AL, Adams JL, Raebel MA et al. Bisphosphonate drug holiday and fracture risk: a population-based cohort study. J Bone Miner Res 2018; 33(7): 1252–9.
Eli Lilly and Company. FORTEO – osteoporosis injection – HCP [Internet]. 2018. Available at WWW: <https://www.forteo.com/hcp>. Accessed September 20, 2018.
Štítky
Biochemie Dětská gynekologie Dětská radiologie Dětská revmatologie Endokrinologie Gynekologie a porodnictví Interní lékařství Ortopedie Praktické lékařství pro dospělé Radiodiagnostika Rehabilitační a fyzikální medicína Revmatologie Traumatologie OsteologieČlánek vyšel v časopise
Clinical Osteology
2020 Číslo 1
Nejčtenější v tomto čísle
- Atypical cases of secondary hyperparathyroidism in patients with kidney disease and failure: case reports
- Guidelines for osteoporotic patients during COVID-19 pandemics
- Effect of anorexia nervosa on bone metabolism
- Management of osteoporosis and calcium metabolism disorders during COVID-19 pandemics


